Understanding Pneumonia: Types, Causes, Symptoms, and More
When it comes to respiratory infections, pneumonia is a common condition that affects millions of people worldwide. It is an inflammation of the lungs caused by various pathogens, such as bacteria, viruses, fungi, or parasites. In this article, we will explore the different types of pneumonia, its causes, symptoms, risk factors, prevention strategies, and treatment options.
Types of Pneumonia
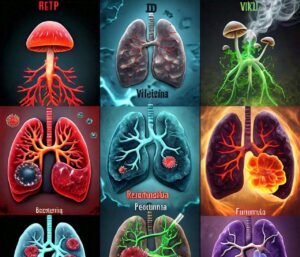
There are several types of pneumonia, which are classified based on various factors such as the causative agent, the setting of acquisition, and the anatomical distribution. Here is an overview of common types:
Based on effective agents:
Bacterial Pneumonia: Caused by bacteria such as Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and others.
Viral pneumonia: Usually caused by respiratory viruses such as influenza, respiratory syncytial virus (RSV) or SARS-CoV-2 (the causative agent of COVID-19).
Fungal Pneumonia: Usually affects people with compromised immune systems. Caused by fungi such as Pneumocystis jirovecii, Aspergillus, and Histoplasma.
Atypical pneumonia: Caused by organisms with unusual characteristics, such as Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumophila.
Based on location and configuration:
Community-acquired pneumonia (CAP): Acquired outside of hospitals or healthcare facilities.
Hospital-acquired pneumonia (HAP): Occurs 48 hours or more after hospitalization, in patients without prior symptoms.
Ventilator-associated pneumonia (VAP): A subtype of HAP that occurs in patients on mechanical ventilation for at least 48 hours.
Healthcare-associated pneumonia (HCAP): Pneumonia in patients who have recently been exposed to healthcare facilities such as nursing homes or dialysis centers.
Based on physical distribution:
Lobar pneumonia: One or more lobes of the lung are involved. It often has a more localized pattern.
Bronchopneumonia: characterized by a complex distribution, affecting multiple areas of the lungs.
Interstitial pneumonia: Affects the interstitial tissue of the lungs, often caused by viruses or autoimmune diseases.
Special categories:
Aspiration pneumonia: Caused by inhalation of food, liquids or gastric contents into the lungs.
Chemical pneumonia: Resulting from inhalation of toxic chemicals or fumes.
Eosinophilic Pneumonia: Characterized by high levels of eosinophils in the lungs, often related to allergies or certain medications.
Each type of pneumonia may require specific treatment methods, and diagnosis often involves clinical evaluation, imaging (such as chest X-ray), and laboratory tests to identify the causative agent. If you have more specific questions or need information about a particular category, i am here to help.
Causes
Pneumonia is an infection that inflames the air sacs in the lungs, causing them to fill with fluid or pus. It can range from mild to severe and can be caused by a variety of pathogens, including bacteria, viruses, fungi, or other organisms. The main causes of pneumonia are:
1. Bacterial Pneumonia:. This is the most common type of pneumonia. The most common cause is Streptococcus pneumoniae (also called pneumococcus), but other bacteria, such as Haemophilus influenzae, Mycoplasma pneumoniae, and Legionella pneumoniae, Can also cause pneumonia.
2. Viral Pneumonia:. This type is caused by viruses such as .Influenza virus., .Sensory syncytial virus (RSV)., .Coronavirus., and others. Viral pneumonia can range from mild to severe, and in some cases, it can lead to bacterial pneumonia as a secondary infection.
3. Fungal pneumonia:. This type occurs when people inhale the spores of a fungus that causes a lung infection. Common fungi that cause pneumonia include .Pneumocystis jirovesi., .Aspergillus., and .Cryptococcus.. Fungal pneumonia is more common in people with weakened immune systems.
4. Aspiration pneumonia:. This occurs when foreign substances, such as food, drink, or vomit, enter the lungs, causing inflammation and infection. This often happens in people who have difficulty swallowing or those who are unconscious.
5. Healthcare-associated pneumonia:. This includes pneumonia acquired in healthcare settings such as hospitals (hospital-acquired pneumonia) or nursing homes (nursing-home-acquired pneumonia). It is often caused by antibiotic-resistant bacteria such as .Staphylococcus aureus (including MRSA). and .Pseudomonas aeruginosa..
6. Ventilator-associated pneumonia:. This is a type of healthcare-associated pneumonia that occurs in people on mechanical ventilation. Ventilator tubes can become contaminated with bacteria, which can lead to infection.
7. Atypical Pneumonia:. This term refers to pneumonia caused by less common organisms such as .Mycoplasma pneumoniae., Chlamydia pneumoniae., and .Legionella pneumophila.. It can have different symptoms and may not respond to the usual antibiotics used for bacterial pneumonia.
Each type of pneumonia may require specific treatment methods, and the severity may vary depending on the cause, underlying health conditions, age, and other factors. If you suspect pneumonia, it is important to seek medical attention for proper diagnosis and appropriate treatment.
Symptoms
Pneumonia is an infection that inflames the air sacs in one or both lungs, which can fill with fluid or pus, causing a range of symptoms. The correct presentation may vary depending on the cause, severity, and the individual’s age and health. Some common symptoms of pneumonia are:
Cough:. Often persistent and may produce phlegm or phlegm, which may be clear, yellow, green, or even bloody.
Fever:. Usually high, but not always.
Chills and chills:. often accompanied by fever.
Shortness of breath:. Difficulty breathing or feeling short of breath with minimal activity.
Chest Pain:. May be sharp or stabbing, often worse with deep breathing or coughing.
Fatigue:. A general feeling of tiredness or lethargy.
Sweating:. Profuse sweating or sweating.
Decreased appetite:. Decreased desire to eat.
Nausea or Vomiting:. Some individuals may experience these symptoms.
Confusion or changes in mental status:. More common in older adults.
In children, symptoms may be more subtle and may include:
Rapid breathing:. Significant increase in breathing rate.
Flaring of nostrils:. indicates difficulty in breathing.
Blue lips or fingernails:. A sign of low oxygen levels.
Lethargy:. Extreme tiredness or lack of energy.
Wheezing or wheezing sounds:. indicates respiratory distress.
If you suspect you or someone else has pneumonia, get medical attention right away. Early diagnosis and treatment are essential to avoid complications.
Diagnosis

The diagnosis of pneumonia involves a combination of clinical evaluation, patient history, physical examination, and various diagnostic tests. Pneumonia is an infection that inflames the air sacs in one or both lungs, which can fill with fluid or pus, causing symptoms such as cough, fever, chills, and difficulty breathing. Here is an overview of the diagnostic process for pneumonia:
1. Patient History:
The health care provider will ask about your symptoms, their duration, and whether you have any risk factors (such as smoking, chronic illness, or exposure to someone with a respiratory infection). .
They will also ask about your medical history, medications, allergies, and recent travel.
2. Physical Examination:
The health care provider will listen to your lungs with a stethoscope for abnormal breath sounds, such as crackles, wheezing, or low breath sounds in specific areas.
They can also check your temperature, pulse, oxygen saturation, and other vital signs.
3. Diagnostic Tests:
Chest X-ray:. This is a primary tool for diagnosing pneumonia. It may show areas of lung inflammation or consolidation.
Blood tests:. These can show signs of infection, such as an increased white blood cell count, and help assess the severity of the condition.
Sputum Culture:. This test involves examining a sputum sample to identify the type of bacteria or other pathogens causing the infection.
Pulse Oximetry:. This non-invasive test measures the oxygen saturation in your blood to determine if your lungs are supplying enough oxygen.
Arterial Blood Gas (ABG):. In more serious cases, this test measures the levels of oxygen and carbon dioxide in your blood.
Additional Tests:. Depending on the severity and underlying cause, additional tests such as a CT scan, bronchoscopy, or specific tests for viral or unusual bacterial infections may be used.
4. Special Considerations:
If you have risk factors such as a weakened immune system, chronic health conditions, or recent surgery, your healthcare provider may perform additional tests to ensure an accurate diagnosis.
Pediatric and elderly patients may require a more detailed examination and additional tests due to their unique health concerns.
Abstract:
To diagnose pneumonia, healthcare providers use a combination of physical examination, chest X-rays, and various laboratory tests to identify the cause of the infection and assess its severity. If you are experiencing symptoms consistent with pneumonia, it is important to seek medical attention immediately for an accurate diagnosis and appropriate treatment.
Treatment

Pneumonia is a respiratory infection that inflames the air sacs in the lungs, which can fill with fluid or pus, causing symptoms such as cough with mucus, fever, chills and difficulty breathing. The treatment regimen depends on the type of pneumonia, the severity of symptoms, the patient’s age, overall health, and other underlying conditions. Here’s an overview of common pneumonia treatment strategies:
1. Clinical Diagnosis:
Pneumonia is diagnosed by a combination of medical history, physical examination, chest x-ray, and laboratory tests (such as sputum cultures and blood tests).
The cause of pneumonia is determined (bacterial, viral, fungal, or other) to guide treatment.
2. Antibiotics:
Bacterial pneumonia is usually treated with antibiotics. The choice of antibiotic depends on the specific bacteria causing the infection, the patient’s age, allergies and other health factors.
Common antibiotics include amoxicillin, azithromycin, clarithromycin, and fluoroquinolones.
For more severe cases, hospitalization with intravenous (IV) antibiotics may be necessary.
3. Antiviral drugs:
If the pneumonia is caused by a virus (such as influenza or respiratory syncytial virus), antiviral drugs such as oseltamivir may be prescribed. However, antibiotics are ineffective against viral pneumonia.
4. Antifungal drugs:
Fungal pneumonia requires antifungal medications. The type of antifungal medication depends on the fungus causing the infection.
5. Management of symptoms:
Fever can be controlled with antipyretics such as acetaminophen or ibuprofen.
Cough suppressants or expectorants can be used, but sparingly, as coughing helps clear the lungs.
6. Supportive Care:
Rest and hydration are important. Drinking fluids helps keep mucus in the lungs thinner and easier to expel.
Supplemental oxygen or breathing assistance may be needed in severe cases or for those with underlying respiratory conditions.
7. Hospitalization:
In severe cases, or in people with weakened immune systems or significant comorbidities, hospitalization may be required for more intensive treatment and monitoring.
Intensive care and mechanical ventilation may be necessary in extreme cases.
8. Prevention:
Vaccination can reduce the risk of pneumonia. Common vaccines include the pneumococcal vaccine and the influenza vaccine.
Good hygiene, hand washing, and avoiding smoking can also help prevent pneumonia.
9. Follow-up and recovery:
Follow-up visits with a health care provider to make sure the infection is resolving and to address any lingering symptoms or complications.
Recovery times vary, but many people start feeling better within a few days to a week, with full recovery taking a few weeks or longer, depending on the severity of the infection.
Get medical help right away if you suspect you have pneumonia or have severe symptoms such as chest pain, difficulty breathing, or a high fever. This is especially important for young children, the elderly, and people with weakened immune systems.
Risk Factors
Pneumonia is an infection of the lungs that can be caused by bacteria, viruses or fungi. It causes inflammation in the alveoli (small air sacs in the lungs), which can fill with fluid or pus, causing symptoms such as cough, fever, chest pain, and difficulty breathing. There are several risk factors that increase a person’s susceptibility to pneumonia. These risk factors may vary depending on age, health conditions, lifestyle and other factors. Here is an overview:
1. Age:
Very young children (especially under 2 years old) and older adults (especially over 65 years old) are at higher risk of pneumonia.
2. Weak immune system:
Conditions such as HIV/AIDS, cancer, autoimmune diseases, and the use of immunosuppressive drugs can weaken the immune system, increasing the risk of pneumonia.
3. Chronic health conditions:
People with chronic conditions such as chronic obstructive pulmonary disease (COPD), asthma, heart disease, diabetes, or chronic kidney disease are at higher risk of developing pneumonia.
4. Smoking and substance abuse:
Smoking damages the lungs and affects the immune response, making it easier to catch infections. Excessive alcohol consumption may also increase the risk.
5. Respiratory infections and conditions:
Recent respiratory infections such as flu, bronchitis, or colds can increase the risk of pneumonia. Conditions such as cystic fibrosis also increase the risk.
6. Hospitalization or recent surgery:
Hospitalization, especially when it involves mechanical ventilation, and recent surgery, especially of the chest or abdomen, may increase the risk of hospital-acquired pneumonia.
7. Environmental Exposure:
Air pollution, occupational hazards (such as inhaling toxic fumes or dust), or living in crowded or unsanitary conditions can increase the risk of pneumonia.
8. Poor nutrition and hygiene:
Poor nutrition weakens the immune system. Poor hygiene, especially inadequate hand washing, can facilitate the spread of infection.
9. Neurological Disorders:
Conditions that impede swallowing or cause aspiration (eg, stroke, dementia, or neurological disorders) can increase the risk of pneumonia caused by inhaling food or liquids into the lungs.
10. Stay in group settings:
Residents of long-term care facilities or nursing homes are at higher risk due to close living conditions and possibly weakened immune systems.
Understanding these risk factors can help identify individuals who may be at increased risk of pneumonia, preventive measures such as vaccinations (eg, flu vaccine, pneumonia vaccine), lifestyle changes (eg, quitting smoking). and better hygiene practices. If you have concerns about pneumonia or its risk factors, it’s best to consult a health care provider for personalized advice and prevention strategies.
Preventions

Pneumonia is an infection that inflames the air sacs in one or both lungs. Prevention focuses on reducing risk factors and strengthening the body’s defenses. Here are some important strategies to help prevent pneumonia:
1. Vaccination:
Get vaccinated against pathogens that cause pneumonia. The most common vaccines are for pneumococcal bacteria and Haemophilus influenzae type b (Hib).
Get an annual flu vaccine. Influenza can cause pneumonia, especially in high-risk groups.
2. Practice Good Hygiene:
Wash your hands regularly with soap and water, especially after coughing, sneezing, or touching potentially contaminated surfaces.
Use hand sanitizer when soap and water are not available.
3. Avoid Smoking:
Smoking damages lung tissue and reduces the respiratory system’s ability to fight infection. Avoid smoking and exposure to secondhand smoke.
4. Maintain a healthy lifestyle:
Eat a balanced diet rich in fruits, vegetables and whole grains to support your immune system.
Exercise regularly to maintain good lung health and circulation.
Get adequate sleep to support your body’s natural defenses.
5. Manage chronic conditions:
If you have chronic conditions such as diabetes, asthma, or chronic obstructive pulmonary disease (COPD), work with your healthcare provider to effectively manage them.
6. Minimize respiratory infections:
Avoid close contact with sick people, especially if they have respiratory symptoms such as coughing or sneezing.
If you are sick, stay home to prevent spreading the disease to others.
7. Keep indoor air clean:
Use air purifiers to reduce indoor air pollution and ensure proper ventilation in your home.
Minimize exposure to environmental pollutants such as smoke, dust and chemicals.
8. SEEK MEDICAL ATTENTION FOR RESPIRATORY SYMPTOMS:
If you develop symptoms such as a persistent cough, fever, chest pain, or difficulty breathing, seek medical attention immediately. Early treatment can help prevent complications.
9. Travel Precautions:
If traveling, stay up-to-date on vaccines and take precautions to avoid respiratory infections, especially in crowded or high-risk environments.
10. Stay Hydrated:
Drink plenty of fluids to keep mucus membranes moist, which helps protect against respiratory infections.
By following these precautions, you can reduce your risk of getting pneumonia. If you have questions about your specific risk factors or need guidance about vaccinations, consult a health care professional.
Conclusion
Pneumonia is a serious respiratory infection that can affect individuals of all ages. By understanding the different types, causes, symptoms, risk factors, and prevention strategies, you can take proactive steps to protect yourself and reduce the likelihood of developing pneumonia. If you experience symptoms or have concerns, consult with a healthcare professional for a proper diagnosis and appropriate treatment.
